Abstract
Background
Developments in related haploidentical hematopoietic stem cell transplantation (haplo-HSCT) have made two immune systems with incompatible human leukocyte antigens (HLA) adaptable, greatly reducing transplantation-related toxicity. In the haploidentical transplantation system, patient-specific HLA antigens are a primary way in which donor immune cells exert their graft-versus-leukemia effects by alloreactivity, and therefore patient-specific HLA genomic loss is often considered a mechanism of leukemia relapse. Although the incidence and characteristics of HLA loss have been investigated in patients with myeloid leukemia who relapsed after transplantation, patient-specific HLA genomic loss in lymphoid conditions and under different transplantation regimes remain enigmatical. We herein provide the data for HLA loss relapse in lymphoid disease, as well as offer data in myeloid disease based on antithymocyte globulin (ATG) T-cell-replete conditioning.
Methods
Between May 2012 and May 2021, 106 patients were enrolled in this study, including 104 had hematological relapse and 2 had minimal residual disease (MRD) recurrence after haplo-HSCT. All data were collected from centers within the Zhejiang Provincial Workgroup of HSCT. Firstly, the patients were divided into two groups according to the type of disease: myeloid and lymphoid conditions, and secondly, they were divided into the Classic Group and the Loss Group according to whether the patients had unshared HLA genomic loss at the time of relapse or not. A two-tailed P value of 0.05 was considered statistically significant. Univariate analysis is performed using the χ2 test, Fisher exact test, and Student t test, as appropriate. A multivariate model was used to calculate the odds ratio (OR) with a 95% confidence interval (CI). Post relapse overall survival (prOS) was estimated and plotted using the Kaplan-Meier method.
Results
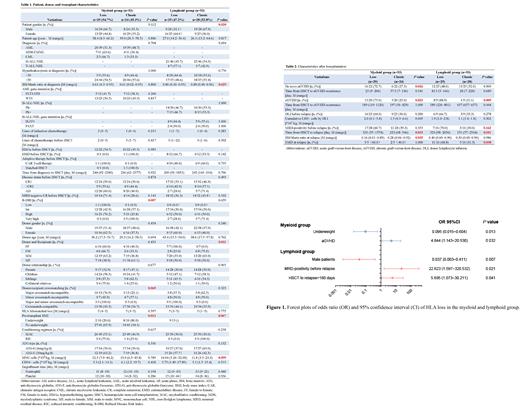
Of all patients, HLA loss was detected in 50.9% (54/106) patients and the occurrence was not related to disease type (P=0.44). Patients having either myeloid malignancies or lymphoid malignancies with HLA loss experienced relapse later than those with classic relapse. The demographic and baseline characteristics of patients were summarized in Table 1, and the post-relapse parameters were presented in Table 2.
We next determined what factors correlating with HLA loss at relapse by multivariate analysis. For patients with myeloid malignancies, a pre-transplant underweight status based on body mass index (BMI) was a factor strongly correlated with classic type when relapse (OR=0.095, 95%CI: 0.015~0.604, P=0.013); patients suffering de novo aGVHD had an OR of 4.844 (95%CI: 1.143~20.530, P=0.032) (Figure 1). As for lymphoid conditions, patients who experiencing MRD-positivity before hematological relapse (OR=22.623, 95% CI: 1.597~320.532, P=0.021), and >180 days from HSCT to relapse (OR=5.695, 95% CI: 1.073~30.211, P=0.041) were more likely to lose unshared HLA at relapse. Yet male patients (OR=0.037, 95% CI: 0.003~0.411, P=0.037) were inclined to have classic one when relapse (Figure 1).
For prognosis, in patients with myeloid conditions, the median prOS was 217 days and 215 days in the Loss Group and Classic Group, respectively (P=0.34). In the Loss Group, the white blood cell (WBC) at diagnosis was related to prOS (>50ⅹ10 9/L vs. ≤50ⅹ10 9/L: median: 157 vs. 261 days, P=0.037). For patients having male donors, patient gender was related to prOS: median prOS was 386 days for male patients and 124 days for female patients (P=0.008). For patients with lymphoid malignancies, the median prOS was 285 days and 244 days in the Loss Group and Classic Group, respectively (P=0.24). The results of the univariate analysis from the Loss Group showed that male patients (median: 40 vs. 194 days; P=0.036) and cGVHD fare (median: 114 vs. 468 days; P=0.002) were related to inferior prOS.
Conclusion
The occurrence of patient-specific HLA genomic relapse after haplo-HSCT appears later than classic relapse. In myeloid malignancies, the patient pre-transplant BMI and aGVHD fare are associated with the relapsed type. In lymphoid conditions, patient sex, presence of MRD-positive results before relapse, and the time from transplantation to relapse correlate with HLA loss at relapse. Yet this study is based on a limited number of patients, further validation in other centers is warranted.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal